What matters about atherosclerosis? Uncontrolled inflammation in the intima.
What inflames the intima beyond control? The reaction to unwanted cholesterol and LDL particles getting into the intima. The reaction involves white blood cells entering from the bloodstream, then turning various immune cells like dendritic cells and macrophages. Some of these become “foam cells” after absorbing the unwanted particles. Recent evidence points to a functional role for DCs in all stages of atherosclerosis because of their myriad functions including lipid uptake, antigen presentation, efferocytosis, and inflammation resolution.
This process becomes a problem because cells increase in number faster than they leave the intima. This leads to “plaque” buildup, promoted by the response to foam cell presence and death. Plaque is a combination of several molecules and includes immune and muscle cells. It was previously thought that plaque could only increase over time, and that we never “lost” it. However, during the 1980s, Badimon et al (21) showed that plaque development is a dynamic process that can be slowed, stopped or reversed. Source paper
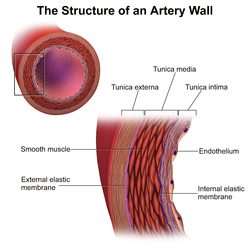
What recruits macrophages? The epithelial cells which line the inside of blood vessels. They call for white blood cells to deal with oxidized and non-ox LDL that have entered the intima. They’re especially reactive to ox-LDL.
What causes LDL to reach the intima?
The entry of LDL into the arterial wall (in moles of LDL per surface area per unit of time) has two major determinants: the LDL concentration in plasma and the arterial wall permeability. LDL enters the arterial wall as intact particles by vesicular ferrying through endothelial cells and/or by passive sieving through pores in or between endothelial cells. Estimates in vivo of the LDL permeability of a normal arterial wall vary between 5 and 100 nl/cm’/h. In laboratory animals, the regional variation in the arterial wall permeability predicts the pattern of subsequent dietary induced atherosclerosis. Moreover, mechanical or immunological injury of the arterial wall increases the LDL permeability and is accompanied by accelerated development of experimental atherosclerosis. This supports the idea that an increased permeability to LDL increases the risk of atherosclerosis. Hypertension, smoking, genetic predisposition, atherosclerosis, and a small size of LDL may all increase the arterial wall permeability to LDL and in this way increase the risk of accelerated development of atherosclerosis.
Also, Macrophages eat LDL, keep TG, and send cholesterol out via nascent HDL. Excess cholesterol remains and forms crystals in lysosomes. Enrichment of ER membranes with free cholesterol can result in defective cholesterol esterification by ACAT in macrophages favoring further accumulation of free cholesterol. Also, free cholesterol enrichment of cell membranes can enhance inflammatory signalling from lipid rafts, particularly TLR signalling and activation of nuclear factor-κB (NF-κB) 41–43. Furthermore, trafficking of free cholesterol out of lysosomes may also become defective in these macrophages, constituting a barrier to cholesterol efflux and further amplifying inflammation.
What oxidizes LDL? NEED TO READ
- Inside intima: ROS from Monocytes?
- How do monocytes get inside? Recruited by epithelium due to irritants.
- In bloodstream: by ROS. It is generally assumed that ox-LDL present in the arterial intima is derived from LDL particles that have been modified within the arterial wall.2 This concept that oxidation primarily occurs extravascularly is supported by the finding that addition of plasma inhibits cell-induced oxidation of LDL,2 an effect presumably due to the presence of antioxidants in plasma. Furthermore, extensively ox-LDL is removed rapidly from plasma immediately after intravenous injection.11 12 Other studies suggest, however, that as much as 10% of LDL in plasma may be oxidized.13 14
- Before bloodstream: Can be oxidized before being packaged as VLDL (e.g. cooking, rancidity).
126. Staprans I, Rapp JH, Pan XM, Hard-man DA, Feingold KR. Oxidized lipids in the diet accelerate the development of fatty streaks in cholesterol-fed rabbits. Arterioscler Thromb Vasc Biol. 1996;16:533–538.[PubMed]
How does the LDL get there? Normal lipid metabolism. (transcytosis)
- Epithelium disfunction?
- What causes that? Smoking, hypertension, # normal LDL, oxLDL, high glucose, LDL undergoes post-translational modifications while in circulation such as oxidation.
- Something about Apo B100?
- More LDL P to bump into epithelium?
-
- What increases LDL p? VLDL synthesis.
- What increases VLDL synthesis?
- What increases LDL p? VLDL synthesis.
- Full hepatic glycogen?
- How much is full?
- Need to transport cholesterol to cells?
- What causes need?
- Macronutrient ratio?
- Hormones (insulin, glucagon, epinephrine)?
Do we understand enough to try stuff?
Do more TG get made from carbs or fat?
How are protein turned into TG?
How is alcohol turned into TG (is it the alcohol or the sugar in the drink)?
How is glycogen made?
Is cholesterol a lipid?
What diglycerides aren’t absorbed by duodenum?
a clear relationship between the glycemic index of a meal and its ability to stimulate de novo lipogenesis awaits further study.
Glucagon inhibits ACC but supports glycogen breakdown. So how to raise glucagon would be good for reducing FA synthesis, and reducing TG formation and subsequent VLDL creation.
Triplet oxygen is the most common oxygen isotope.
Food oxidation Hydrogen at C11 of linoleic acid is removed at 50 kcal/ mol. The energy required to remove hydrogen in C8 and C14 of linoleic acid is 75 kcal/ mol and the homolytic dissociation energy between hydrogen and C17 or C18 is about 100 kcal/mol (Min and Boff 2002).
Citrate and insulin upregulate Acetyl CoA Carboxylase, glucagon and epinephrine downregulate ACC
Long term regulation is that carb +ATP upregulates, fats/starvation downregulate
Enterocyte lipid absorption to chylo export:
High vs low fat meal absorption
Carbs packaged as TG by enterocyte
FYI: Protein vs carb absorption and export by enterocyte
Academic page on cholesterol and lipids
Important distinction: endogenous lipid transport
Metal activation, enzyme catalysis or photooxidation: Less energy is required
Oxidation Inhibited by tocopherols, mannitol and formate